Stemming the tide in the north

A pilot scheme aimed at stemming the damage methamphetamine is causing in Northland has reached the 12-month milestone.
Te Ara Oranga was allocated $3 million for extra treatment, more Police and community-led prevention activities with an emphasis on people working collaboratively across Te Tai Tokerau. A short extension has been granted after a progress report delivered to the government in June is reviewed. Those involved are adamant Te Ara Oranga has proved its worth and should continue.
Keri Welham travelled to Northland to see what Te Ara Oranga has achieved in its short life and how other communities across New Zealand could use this model.
When Kevin* wanted to finally break 15 years of daily meth use, he moved to Northland. That was five years ago. These days, that’s the last place you’d go to escape meth.
The drug has its hooks in Te Tai Tokerau. Wastewater analysis indicates higher meth use in Whāngārei than in any other city or town in New Zealand.
Kevin* ... thinks he might have given up years earlier if a GP had talked to him about treatment options and a support worker had called offering to walk the journey with him. He could have been spared years of pain.
An innovative one-year pilot has sought to reduce the chaos meth is causing up north. Te Ara Oranga [see sidebar] has brought together Police, Health, NGOs and residents – a community working together to address a problem and develop tailored solutions. The pilot is nearing completion, and many say it has been a game changer.
Kevin is a huge supporter of Te Ara Oranga. He thinks he might have given up years earlier if a GP had talked to him about treatment options and a support worker had called offering to walk the journey with him. He could have been spared years of pain.
Kevin is now a business owner and a support worker with the Ngāti Hine Health Trust – the same organisation that gave him life-changing residential treatment when he arrived in Northland.
He lives in Kaikohe and estimates “at least” 20 percent of the town’s 4,000 residents are using meth. He claims it’s a similar picture in Moerewa, Kawakawa and most of Northland’s other small rural towns.
Recently, a man came in to his shop to buy treats for his children. His bank card was declined, and Kevin said the man could have the ice creams and pay him back another day. As the man fumbled to put his card back in his wallet, a bag of meth fell onto the counter. The man was quick to reassure that he was only using “part-time”. Kevin briefly and gently outlined his lived experience and the services in their town, including the boosted support available through Te Ara Oranga.
A week later, the man came back and asked Kevin for help.

Wayne Whitney, Ivy Tenana, and Darin Goodwin promoting ‘Te Ara Oranga’ at Waitangi in February 2018. Photograph by Michael Cunningham for The Northern Advocate.
Northland stretches from southeast of Mangawhai across to the Kaipara Harbour and all the way up to New Zealand’s northernmost tip, Cape Rēinga. The region spans 13,286 square kilometres, has 10 harbours and is home to 165,000 people – almost 85,000 of them in Whāngārei.
In tiny Moerewa (population 1,400), you can buy pork bones and watercress at roadside shops. A grown man rides a tiny BMX in gumboots, beefy dogs roam, cacti grow, lawns are tight clipped on some sections and tractors decay on others. In the drizzle, a man walks down the street, hood up, fighting vigorously with his jacket pockets as though trying to free himself. One home has rotting weatherboards and no curtains, and from the road, you can see a single mattress on the ground. Many other homes seem to be disintegrating in the damp tropical warmth, melting into the earth. A fairly new car seat lies in a sopping wet driveway. On the main street, men in white AFFCO gumboots walk into the bakery.
State Highway 12 passes the Northland Region Corrections Facility, and then you’re in Kaikohe. It’s a service town where you can buy cars, pre-loved clothing, headstones. The Police station roof is covered in lichen. A man struts up and down the main street on a relentlessly wet day holding a small radio, yelling and kicking billboards.
This is a health issue. Substance abuse is a health issue...We [Police] have been disconnected from the health issue. Traditionally, we might have just criminalised everything, but we went out to engage with communities.
Dean RobinsonKevin says he knows of homes in Kaikohe where methamphetamine is being consumed by three generations. He knows of intermediate-age children caught with meth at school.
“The problem in a town like this is people look up to the wrong people.”
He says gang members are viewed as role models, and many people are drawn in by the potential to make a lot of money dealing meth. But, as a former meth user himself, Kevin knows the reality is that it’s highly unlikely individuals will be in the game long enough to get rich dealing a messy, highly addictive, problematic drug like meth.
“There is no one that we know who is retired and living with their millions on an island in the Bahamas.”
A couple of years back, Northland Police and Health began working together on two other critical issues – youth suicide and family violence. They jointly applied for Proceeds of Crime funding to support the Family Harm focus, but Cabinet said it’d like the agencies to look at tackling methamphetamine – the drug that was becoming a regular fixture in family violence, causing a wave of social harm across Te Tai Tokerau.
Police, Health, NGOs and community representatives brainstormed together and came up with the framework for Te Ara Oranga.

Kaikohe Dance Crew with local Police filming the ‘Let’s make a change’ music video in Kaikohe. Photo credit: Liz Inch.
Work to flesh out the programme started with intensive community consultation across Northland, led by community action expert Pam Armstrong. Hundreds attended. Communities were listened to, and their ideas became the basis of some of the most effective elements of Te Ara Oranga.
One example is a cheap, easy-to-distribute fridge magnet. It features the meth cycle – information that is highly valued by families faced with a person who is changing before their eyes. Initially, 1,000 magnets were printed and distributed. They were such a hit, Police funded an additional 5,000.
Another suggestion was to create resource kete to go to each community containing stickers, videos, magnets, billboards. Five of the kete were created, blessed and delivered back to the communities through a second series of hui attended by 600 people.
Throughout the consultation phase, Pam asked people at hui to share their stories.
“The drug’s a terrible thing,” she concluded. “With smoking dak, it’s not problematic. The behaviour’s nowhere near as problematic. They are not ripping people off and doing these out-of-it crimes.”
People exploit their children’s basic needs to extract money for methamphetamine from their families. Many women sell sex to pay off drug debts. Many Northland families have been financially stripped bare by one family member who has lost control. Clinicians say night industry staff use it to stay awake and get hooked. Middle class professionals use it recreationally – and it takes over. On marae, people turn up pre-loaded – their whanaunga take one look at them and know they’re “on the fries”. There’s even talk that it’s swapped by teens at high school in exchange for lunch money.
We talk with users and most suppliers and offer access to treatment programmes. From science, we know [you] can’t always convince people they need treatment.
Dean RobinsonDuring the consultation, many marae requested resources to help them discuss methamphetamine use with members of their hapū.
“They could see their community was starting to be impacted,” Pam says. “They wanted to prepare themselves.”
Across Northland, one-third of residents are Māori. North of Kawakawa, that figure is 43 percent. Roughly 50 percent of clients in alcohol and other drug (AOD) treatment across the region are Māori.
Pam says the high rates of drug use among Māori are a direct link to the poverty in which many Māori live.
“When you don’t have much, you’re willing to take the risks. Poverty goes hand in hand with drug use. It would appear that some of the most vulnerable people are the ones that it’s impacting on more significantly.”
Jenny Freedman is the professional leader of AOD treatment for Northland District Health Board (DHB) Mental Health and Addiction team. She says it was critical Te Ara Oranga was anchored in Māori tikanga.
“You’ve got to match your community,” she says. “You want people’s ears to be open, [for them to] feel as comfortable as they can.”
Recruitment for the new community outreach positions created by Te Ara Oranga was challenging. People had to come from the community, and the contracts were only for one year, so there was no job security. Where possible, the project team worked to attract applicants with experience of living in the towns where the positions would be based, familiarity with te ao Māori and experience living with addiction.
Jenny says Te Ara Oranga has broken new ground in drug harm reduction. One example is an employment programme where people are supported into jobs before they have stopped using. In many instances, this means the job seekers are still committing crimes to fund their use.
Rebecca Priest, an occupational therapist from Workwise employment agency, approached community-centric employers who understood that employment aids recovery and had some tolerance for unreliability and the other issues people using methamphetamine often bring. She helped prepare the job seekers with fresh CVs and meditation techniques to calm anxiety and worked with each job seeker and employer to negotiate appropriate terms.
In total, there were 67 referrals to Te Ara Oranga’s employment programme. Of those, four people who were in danger of losing their jobs were supported to keep them, 26 people obtained new work and eight people undertook vocational training.
Jenny: “We’ve got people with significant criminal histories now in jobs.”
She says the programme has also enabled the DHB to access a whole new swathe of people in need. Of the 308 referred to Northland DHB for treatment in the six months to 31 March this year, 120 were not previously known to mental health and addiction services.
Normally 50 to 60 percent of referrals come from Corrections – people who are forced to seek treatment as part of their sentence. Through Te Ara Oranga, referrals came from Police, GPs, Whāngārei Hospital’s emergency department and other previously untapped avenues.

Ross Smith and Martin Kaipo receive the Whangarei Te Ara Oranga kete from Mare Clarke (right). Photo credit: Liz Inch.
Jenny says people who use methamphetamine are particularly suspicious and paranoid and therefore more help-avoidant than most others who use drugs. On top of this, they tend to be involved in more serious crimes, so often there really are gangs chasing them over debts or issues with dealers.
Jewel Reti project manages the health arm of Te Ara Oranga. She says it can be a very hard drug to identify if you’re not aware of the symptoms. In the beginning, many users lose weight, have energy and look amazing.
“Some will look better than they’ve ever looked,” Jewel says.
It can be a decade before they lose their teeth and are bone skinny – the classic ‘meth look’ from scare tactics campaigns. But by then, they will likely be alone, destitute and living in drug-induced fear.
What if the programme is dropped?
Jenny: “If we only get six months, we won’t get to see the true value of the project.”
What if it is funded, but to a lesser degree. What part of the programme will they drop?
Jewel: “Not one bit of this is any good without all the other bits. That’s the reality of it. You need all the pieces to be effective.”
As a Māori woman living in Whāngārei, Jewel Reti says she has always been a little wary of Police. That has changed since she has come to work alongside Te Ara Oranga’s Meth Harm Reduction team.
Inspector Dean Robinson is Northland’s District Prevention Manager and Police lead for Te Ara Oranga. Jewel helped him recruit his Meth Harm Reduction team, and the Police staff who were handpicked as members were those who displayed empathy for people using drugs and who were comfortable with the pilot’s healthcare approach.
Dean says Te Ara Oranga has changed the mindset for Police, from enforcement towards a healthcare response. His staff say they cannot arrest their way out of a meth crisis, so instead they are referring people to treatment.
“This is a health issue. Substance abuse is a health issue,” Dean says. “We [Police] have been disconnected from the health issue. Traditionally, we might have just criminalised everything, but we went out to engage with communities.”
He realises many New Zealanders would prefer Police locked up all people involved with illegal drugs. But he is convinced of the merits of an approach where officers line up treatment options and support people using drugs and suppliers to get help.
Police have taken what he describes as “a considered approach” to suppliers.
“We talk with users and most suppliers and offer access to treatment programmes. From science, we know [you] can’t always convince people they need treatment.”
So, sometimes charges are used as a tool to get suppliers to engage with treatment – a kickstart, with a clear objective to get the person help. People have told officers they never expected their first offer of help to come from Police. Around 50 percent of those Police have referred for treatment in the past six months were not known to the DHB.
However, Dean is clear Police are not holding back on the organised criminal bodies putting meth onto Northland streets.
“If you are supplying drugs and it’s for the purpose of making money off it and you’re creating a whole lot of harm, we will use the law to intervene,” he says.
Police began testing Whāngārei’s wastewater in August 2017 to establish a baseline against which treatment and enforcement could be measured. If there is a major meth seizure, does the rate of meth in the wastewater fall? Whāngārei wastewater shows population meth use there is currently four times higher than Christchurch and three times higher than Auckland.
In the five months from January 2018, 37 patients were screened for methamphetamine use and provided brief intervention or referral to treatment at 20 different practices.
Back in the early 2000s, Dean and his colleagues started to see methamphetamine hitting the streets of Northland. Police jurisdictions offshore had warned that the drug was highly addictive and, therefore, commonly unleashed a disastrous impact on the lives of people using it.
In the beginning, it was locally manufactured in relatively small batches, and base products were sourced in New Zealand. Consumers then didn’t have a sophisticated knowledge of the drug, so the ‘meth’ they were buying was sometimes more salt and glucose than anything.
At this stage, a point bag (usually 0.1g but not always, depending on supply and demand) was about $100, and at that price, the clientele was largely middle to upper income earners such as truck drivers or business owners.
This began to change as organised criminal groups put more effort into growing demand. Adopting marketing tactics common to shops promoting everyday consumer goods, people were enticed into trying this new drug. A committed clientele for meth began to grow.
At one bust, Police found a whiteboard with a comprehensive operational business plan laid out. It detailed how often the gangs needed to change their delivery routes and how often they needed to buy new phone cards.
Initially, the Police focus was on enforcement – dismantling labs and locking up those involved in manufacture. But the gangs just used their contemporaries’ experiences offshore to find new ways to source methamphetamine and its precursors and to avoid detection. This is when the importation of the drug and its key ingredients really ramped up.
A surge in the availability of methamphetamine means there is barely a corner of the region unaffected. Unlike cannabis, which has long been synonymous with the languid Northland lifestyle, Dean says there is widespread disgust for meth in Northland. “The community absolutely hates it.”
Jenny Freedman agrees.
“The community would tell you it’s massive,” she says. “Everybody you meet has a story.”
Many high-functioning business owners, lawyers, doctors and others with generous incomes and considerable assets are using methamphetamine as are those living in extreme poverty, who don’t have a job or home to lose.
“Initially, it was those who could afford it,” Dean says. “Then, it was those who couldn’t afford it but would do crime to fund it.”
Clinicians have come across kaumātua in the grip of the drug, losing their life savings and their mana. And entire workforces at some small-to-medium Whāngārei businesses are on it, passing around a meth pipe on a Friday night after work in the same way they may once have passed around a joint or sat together drinking beer.
Dean: “We’ve now got a culture of use which has become increasingly normalised.”
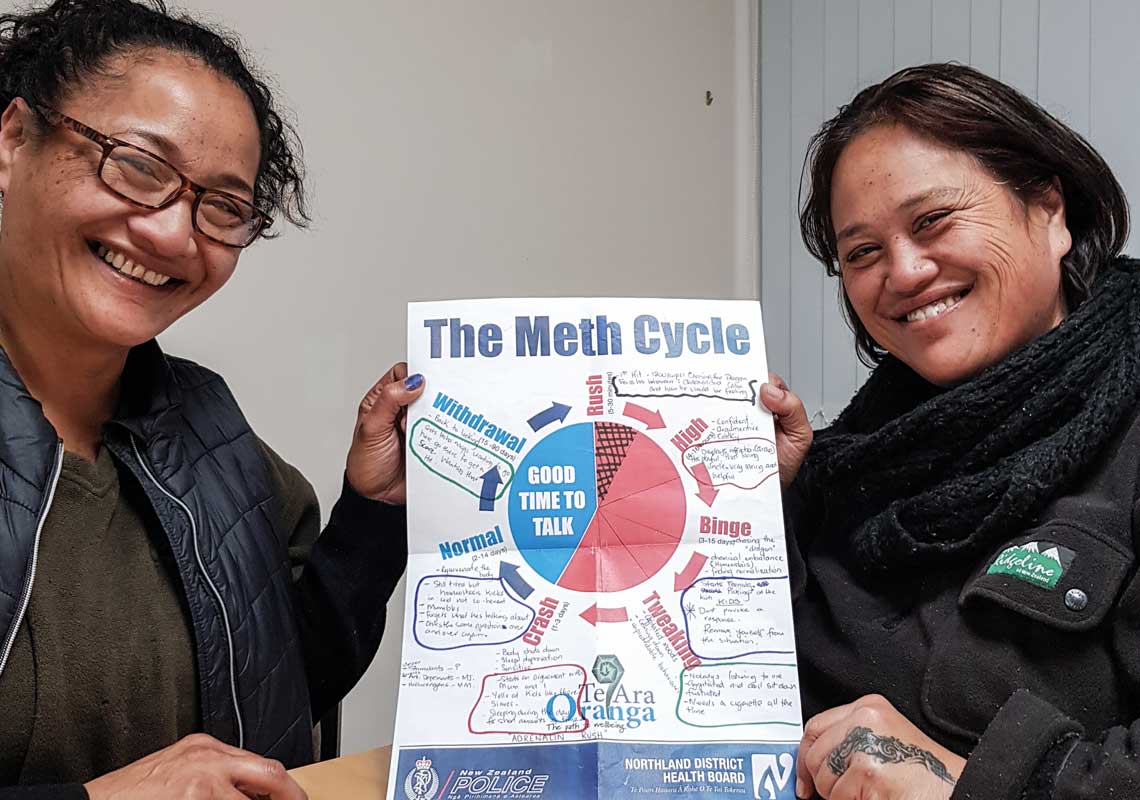
Sisters Gina Rihari-Pedersen and Lovenia Hillman with the meth cycle that’s been useful for their whānau. Photo credit: Keri Welham.
Maurein Betts led development of Te Ara Oranga’s various screening and brief intervention tools for GPs.
Around 60 primary care nurses received fresh training in managing patients with mental health and addiction requirements. Documents about methamphetamine, which GPs could print out and go through with patients, were added to practice databases. Counselling packages were available for GPs to offer patients. Addiction treatment organisations were also added to the GPs’ e-referral system, making it much easier to arrange a referral.
The tools were made available in 40 practices across Northland. In the five months from January 2018, 37 patients were screened for methamphetamine use and provided brief intervention or referral to treatment at 20 different practices. Maurein was delighted with this result. It’s not possible to check, but she suspects there would not have been a single referral from those 40 GP clinics in the year preceding the pilot. This is not about a lack of interest or indifference – it’s about finding time to become familiar with methamphetamine use issues when there is a line out the door and the day is compartmentalised into 15-minute slots.
Recently, in a poorer suburb of Whāngārei, a 19-year-old father of two came to see his GP. He’d been smoking methamphetamine and thought he had some wax stuck in his throat. Staff at the practice were confident in their response. They openly discussed treatment, and when the patient refused, they devised a plan. Without breaching patient confidentiality, they gained kaumātua consent to disseminate generic meth cycle information throughout the wider family so those around him could keep themselves safe.
“For us,” Maurein says, “that’s amazing.”
She says the community will feel betrayed if Te Ara Oranga programmes built on community suggestions – which appear to be helpful in their infancy – are not continued.
“All the places where people might touch patients, we’ve strengthened. A lot of our stuff only really started working four months ago,” she says.
“We often get the pilots, but we don’t get the plane.”
We often get the pilots, but we don’t get the plane.
Maurein BettsSisters Gina Rihari-Pedersen, 49, and Lovenia Hillman, 48, were worried about their brother.
His behaviour had changed markedly. He was a quiet, loving, gentle man with an envied knowledge of tribal customs. He became an angry, threatening, antagonistic dad and uncle. He chucked his job in and walked out on his family.
“He was a totally different man who demanded everybody’s respect and wanted everybody to listen to him,” Gina says. “We were all walking on eggshells.”
Around the same time, Te Ara Oranga came to Kaikohe. A support group was started for families of those using methamphetamine (these support groups were one of the most common requests from communities during development of the pilot).
The sisters didn’t think meth was the issue but agreed some of the kōrero at the support group might be helpful in determining a way forward for their whānau.
A diagram of the meth cycle was shown at the support group, and they stared, nudged each other and shook their heads. Every behaviour outlined was a perfect match for their brother’s new personality. Their brother was on methamphetamine.
The sisters called a meeting with him, his GP, treatment services and their mum. Clearly motivated by a desire to stop hurting his mother, their brother confirmed he was using meth and agreed to treatment.
Meanwhile, the sisters set about writing a whānau safety plan. It outlined when in the meth cycle the children should avoid their uncle and where to go if they had to leave the house because of his behaviour.
Today, in the warm, worn, windowless room where they meet at Mid-North Health and Addiction Services in Kaikohe, they unfold two large sheets of paper and lay them on the table. The first is the meth cycle poster, filled in with words their family had used to describe their brother’s behaviour. The second is their whānau safety plan, including evacuation procedures. These pieces of paper chart this family’s journey.
As well as the knowledge they gained in this room, they also valued the company on what had felt like a lonely journey. Families come from all over the region – some travel for over an hour each way, every Monday night – to be with others facing a similar road. Lovenia says her focus has now moved from being there for her brother, who had not used methamphetamine for three months at the time of writing, to being there for other Kaikohe families.
“I’ve lived here all my life,” Lovenia says, “and they are my whänau and I want to help.”
There is the chance this determined family would have found help in the end, even without Te Ara Oranga. But it would have taken longer to locate, and once they did, the waiting times would have been several weeks longer. During those weeks, more damage would have been done, more people hurt.
Across the car park works Teropu Pou. She is General Manager of Te Hau Ora o Ngāpuhi, which focuses on the wellbeing of children and babies.
She feels used by Te Ara Oranga. She features in the programme’s videos, supported its billboards and was excited to imagine her organisation’s ideas might be used.
She wanted the ability to have a retreat programme where women using methamphetamine could go away, just for a week or two, and have their children come and visit. They’d organise professional guidance for around four women at a time and the kids would be safe – Teropu was going to babysit them herself. All the women involved were specialists prepared to do the work for free.
“It was voluntary. We felt as Māori leaders [that] we needed to contribute back.”
The intention was treatment with a focus on strengthening bonds with children and building resilience and confidence in women. Teropu acknowledges the numbers would have been small but she says the positive outcomes for those whānau would have had far-reaching consequences.
However, her idea was not one of those chosen, and she believes Te Ara Oranga “hasn’t even changed anything” for women and children affected by meth.
Pam Armstrong, who ran the community consultations, says it is valid the community wants to run its own programmes, but the scope was not there for localised initiations in the one-year pilot.
Jenny Freedman from the DHB says building a residential facility to house such a programme would have cost $2 million – the total amount allocated for the health part of the contract.
“We had to make a decision with that money and timeframe, and residential treatment was not viable,” she says.
However, she can see a place for marae-based programmes to cater to ideas such as Teropu’s, as the marae setting doesn’t require the same clinical rigour and hospital-grade facilities that are a necessity when a DHB is involved.
Teropu says everyone in her town has experience with methamphetamine. She says a “wave” is coming for Northland. “How do we stop this thing?”
Te Ara Oranga is the first step, she says. It needs to be continued – and extended.
“I think it’s just the beginning. It’s just touching on it. People are still screaming out for more support. There’s not enough support.
“It’s a start. It’s just a start.”
One of the most desperate needs in Northland is still unmet. The project hoped to increase DHB detox beds in the region from five to seven, to decrease crippling wait times of up to eight weeks for residential treatment.
But building requirements, such as consents to create beds that meet strict healthcare standards, take time. Northland DHB spokesperson Liz Inch says the funding for the beds is locked in and the detox unit extension will be built regardless of whether the pilot is extended.
As they wait to hear about the future of the programme, those involved are moving back to the roles from which they had been seconded and reflecting on this last whirlwind year. Colleagues in other parts of New Zealand are anxious to hear what has worked, what they could repurpose for their region.
Dean says the programmes that make up Te Ara Oranga are a perfect fit for Northland but might not necessarily suit the unique demographics of other communities. A community that was less spread out geographically, with a larger and more ethnically diverse population, might come up with totally different responses to an intruder like methamphetamine.
“This has worked for Te Tai Tokerau,” Jewel says.
Could the same programme be replicated elsewhere?
“A big city might do it differently,” she says. “We’ve got some tools that might work [elsewhere], but you have to adapt it to work for your community.”
* Kevin is a pseudonym for the person we interviewed who requested their true identity not be used.
Recent news

Reflections from the 2024 UN Commission on Narcotic Drugs
Executive Director Sarah Helm reflects on this year's global drug conference
What can we learn from Australia’s free naloxone scheme?
As harm reduction advocates in Aotearoa push for better naloxone access, we look for lessons across the ditch.

A new approach to reporting on drug data
We've launched a new tool to help you find the latest drug data and changed how we report throughout the year.

