Preventing overdose deaths - background paper
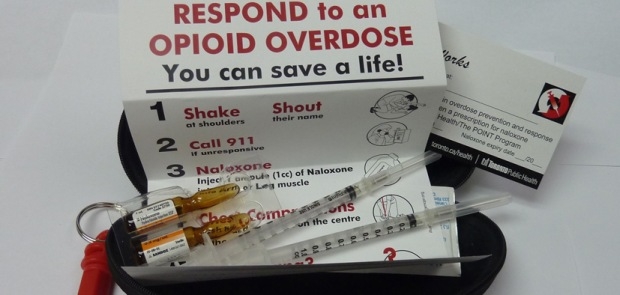
Naloxone kit with instructions
The full paper is available here:
Better emergency overdose interventions are required to reduce the number of preventable deaths in New Zealand. Recommendations for action are included in the Drug Foundation’s background paper on this vital aspect of reducing drug harms. The recommendations were formally adopted by the Drug Foundation’s Board in May 2015.
The position is consistent with a resolution in the Wellington Declaration, accepted in August 2013, calling on the Ministry of Health to “increase the availability of appropriate overdose prevention strategies and relevant services to high risk drug using populations”.
With around 37 deaths per year in New Zealand from opioid overdoses, making up around half of drug related deaths, action to reduce these deaths are needed.
Naloxone is a highly effective opioid antagonist medication which when given to someone who is having an overdose from opioids it stops all the effects of the opioid and can save their life. The drug works in a similar way to adrenalin which is used by people experiencing a severe allergic reaction. It is available as an intermuscular injection in New Zealand and is subsidised by PHARMAC.
Currently only hospitals and some paramedics have naloxone. Internationally naloxone has become a cornerstone of emergency overdose prevention and the three major approaches to make naloxone more accessible are through: non-medical emergency staff such as police having naloxone; pharmacies being able to prescribe naloxone like they do epi-pens; and through take-home kits from needle exchanges after peers train people in overdose prevention. These are not mutually exclusive and any emergency intervention is complementary to longer term overdose prevention provided by drug treatment programs.
Based on international best practice and evidence the Drug Foundation recommends having peer-based training in overdose prevention. Ideally this would be provided by needle exchanges with participants being given take-home naloxone kits. The trainings could be held at the needle exchange premises and through outreach to prisons and treatment centres, covering the groups most vulnerable to overdose.
Additionally naloxone should be reclassified as a pharmacist only medication that is carried by all ambulances and paramedics. Alternatives methods of administration such as a nasal spray should be investigated, alongside non-medical emergency services having naloxone. Increasing access to naloxone can be extended to begin to address the rising concern around overdoses from prescription drugs.
These recommendations were agreed on after the Drug Foundation received input from the Needle Exchange, Capital and Coast DHB Addictions Service, St John Ambulance, Matuaraki Consumer Leadership Group, CADS Consumer Advisory Group and a Clinical Treatment lecturer.
Recent news

Reflections from the 2024 UN Commission on Narcotic Drugs
Executive Director Sarah Helm reflects on this year's global drug conference
What can we learn from Australia’s free naloxone scheme?
As harm reduction advocates in Aotearoa push for better naloxone access, we look for lessons across the ditch.

A new approach to reporting on drug data
We've launched a new tool to help you find the latest drug data and changed how we report throughout the year.

