Overdose prevention: A walk in the park?

Want to help get naloxone out there? We need your donation.
The Drug Foundation has set up a Givealittle to help fund the distribution of naloxone to mark International Overdose Awareness Day, Tuesday 31 August.
Naloxone is a low-risk medication that saves lives. In British Columbia it's being handed out at community training events, and US-based Health Affairs Journal says it should be available over-the-counter. Russell Brown has been watching as the world wakes up to the benefits of the overdose-prevention medication.
In Chilliwack, they made it a picnic.
One fine Saturday last month, the Chilliwack Overdose Prevention Society and Moms Stop the Harm invited the public to come to the Canadian city's Salish Park to learn to save lives. From a line of tables set up by the duck ponds they provided free naloxone kits, training in how to use them – with bags full of oranges to practice injecting on – and a barbecue lunch.
The event is part of a broader move to mobilise against a catastrophic rise in opioid overdoses in the province of British Columbia. Between January and May this year there were 851 opioid overdose deaths in BC. Most of them, 85%, involved fentanyl, which is turning up not only in illicit heroin, but in cocaine. A further 75 were linked to illicit carfentanil, an even stronger synthetic opioid used to tranquillise large animals such as elephants. This year, a new synthetic opioid, Furanyl UF-17, about which almost nothing is known, has been turning up in both police and community testing.
Chilliwack OPS, part of a national network of overdose prevention groups, has also offered pop-up training at local public housing projects and helped deliver an online version of a training course called Not Just Naloxone, created by the First Nations Health Authority. The underlying rationale across all of them is the same: the people most likely to be able to prevent an accidental overdose becoming a fatality are the people around the users – which is usually their friends and family.

A woman watches as another person uses a syringe on an orange. - In Canada, the Chilliwack Overdose Prevention Society and Moms Stop the Harm handed out free naloxone kits and trained people in how to use them. Photo: The Chilliwack Progress.
Sometimes, however, the nearest person is a stranger. Canada's public broadcaster the CBC recently reported the story of Conall MacLellan, who was riding his bike through downtown Edmonton, Alberta, when he saw an unconscious man in the street. He stopped, called 911 and told the call centre he had a naloxone kit and was about to use it. As he had been taught at a recent community training session in his inner-city neighbourhood, he jabbed the unresponsive man in the leg. Within a minute or two, the man was conscious and moving.
That MacLellan is 14 years old and knew what an overdose looked like because he'd seen them before is a confronting fact. But because he had the means and training, he saved a life.
Canadian authorities have been obliged to do a lot of confronting in the past few years. In British Columbia, naloxone is available over the counter and – in the wake of a successful trial last year – drug users can now obtain opioids in several different forms on prescription. The province's Addictions minister Sheila Malcolmson confirmed the new prescription policy last month, saying it would "help to separate more people from the poisoned [street] supply and to help them connect with support and to stabilise their lives."
It might seem a long way away from any New Zealand experience, but peer workers at the New Zealand Needle Exchange Programme have naloxone stories too.
One account from a NZNEP worker provided to Matters of Substance tells of a young woman who came to an exchange for needles for her aunt, who was coming to stay with her.
Her auntie's partner had an overdose and they were able to administer naloxone ... the time delay could have easily been the difference between life and death."
NZNEP worker"After talking for a bit she said she was very concerned as her auntie had overdosed a few years prior at her house and had to be taken to hospital. I told her that I could give her a naloxone kit that she could use to reverse an overdose if it happened again. She gladly accepted it and I gave her a brief demo and instructions on how to use it, what’s included.
"She came back in a few weeks later to thank me for the kit, as her auntie's partner had an overdose and they were able to administer naloxone after his breathing had slowed, his lips were blue and they couldn’t shake him awake. I’m not sure if they still called an ambulance but he was very close to stopping breathing entirely and was bought back by the naloxone less than a minute after it was given. I feel this was an excellent outcome as even with an ambulance attending, the time delay could have easily been the difference between life and death."
Two other stories from the NZEP frontline involved a group in which opioid use may be on the rise: students. In one case, a young woman who was part of a camping group that had packed a substantial supply of alcohol and drugs was found unresponsive in her tent. She was brought back with naloxone administered by a nurse who was camping with them. It took two injections before she regained consciousness. In another incident, a PhD student studying what the worker recalled as "something to do with chemistry" found a friend overdosing on fentanyl. It took three naloxone injections to bring him back.
There will not always be a nurse or a budding chemistry PhD at hand, but in all three cases, there was a common factor: naloxone and the basic training to use it in an emergency.
The benefits of putting naloxone into the hands of those most likely to encounter an overdose are increasingly being recognised in other places. Police officers in several Scottish districts, for example, were this year offered the option of carrying naloxone in spray form on their utility belts. The pilot project, funded by the Scottish government's Drug Deaths Taskforce, was developed in consultation with people with lived experience of naloxone.

The officers are trained to use naloxone, but aren't expected to provide full emergency medical care. While naloxone is generally harmless if mistakenly administered to someone not suffering an opioid overdose, it can have the effect of putting someone already dependent on opioids into abrupt withdrawal, which has medical implications. (Medsafe's consumer information sheet, for example, emphasises that it is an emergency medicine and "you must get emergency medical attention as soon as possible after its use.") But if the officer on the scene can get someone revived and stabilised while an ambulance is on the way, that is potentially a life saved.
It's not all good news. While Canada is moving swiftly, across the border in US, access is patchy and difficult in some of the places where overdose deaths are most critical. And that's two years after the US Surgeon General published an advisory declaring that for "family and friends of people who have an opioid use disorder, and community members who come into contact with people at risk for opioid overdose, knowing how to use naloxone and keeping it within reach can save a life."
The journal Health Affairs last month examined the obstacles to access in American cities – from racism and stigma to a simple lack of pharmacies in some neighbourhoods – and recommended naloxone be reclassified as an over-the-counter medicine, much as emergency contraception was more than a decade ago.
"The drug’s benefits outweigh its risks, it treats a condition that can be identified without a medical professional’s guidance, it has a low misuse potential, and the instructions are understandable by a layperson," wrote Health Affairs' authors.
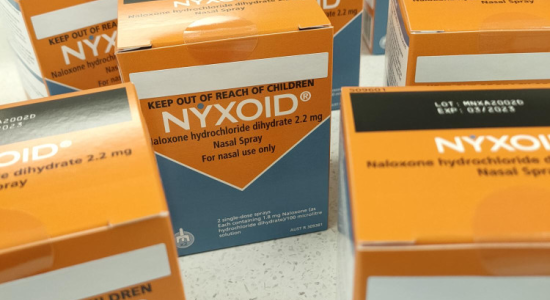
In New Zealand, naloxone is available in both injectable form and as the Nyxoid nasal spray, but access to it is complicated in some of the same ways as it is in America. It's not a given that New Zealand will continue to avoid the same catastrophic adulteration of street drug supplies that the US and Canada are are grappling with. It would seem to be worth doing the thinking about improving access to naloxone now, rather than later.
Header Image by The Chilliwack Progress.
Recent news
Expert Pharmac committee recommends funding for overdose reversal nasal spray
Public funding for a lifesaving opioid overdose reversal nasal spray is one step closer, with an expert committee saying that funding the medicine for use by non-paramedic first responders and people at high risk of an opioid overdose is a

Reflections from the 2024 UN Commission on Narcotic Drugs
Executive Director Sarah Helm reflects on this year's global drug conference
What can we learn from Australia’s free naloxone scheme?
As harm reduction advocates in Aotearoa push for better naloxone access, we look for lessons across the ditch.

