'Grossly underprepared' - NZ's naloxone mess

Want to help get naloxone out there? We need your donation.
The Drug Foundation has set up an ongoing Givealittle to help fund the distribution of naloxone.
So far, New Zealand has escaped the kind of opioid crisis that has claimed thousands of lives overseas. But should that change, experts warn we are “grossly underprepared”. Catherine Masters investigates what’s holding up the supply and distribution of the overdose reversing medication naloxone.
New Zealand appears not much closer to getting widespread availability and distribution of the lifesaving drug naloxone, which reverses opioid overdoses, despite years of lobbying by agencies and harm reduction experts, and efforts from the Ministry of Health.
Experts say opioid overdoses already claim at least 40 lives a year in this country, and there is a risk Aotearoa could face an opioid crisis like the ones being experienced in North America and Europe.
“Overseas we are seeing tens of thousands of deaths, caused largely by prescription opioids, heroin and adulteration of other drugs like MDMA and methamphetamine with a powerful opioid called fentanyl and its analogues,” says the Drug Foundation’s executive director, Sarah Helm.
She says that here in Aotearoa we risk a similar situation emerging without the capacity to respond in time because of a lack of naloxone availability. Recent reports of a local increase in home bake heroin also add urgency to the issue.

Hyundai sedan with yellow St Johns ambulance signage drives past lit-up shops on a dark street at night. Photo: St John - Some St John vehicles staffed by paramedics carry naloxone here in New Zealand, but Police do not.
“Overseas you have widespread take-home emergency naloxone kits for people who use opioids, and first responders like police equipped with them,” says Helm.
Helm says that in Australia, a three year pilot has seen positive results. Naloxone distribution has also meant helpful conversations and relationships have been formed between people who use drugs and the pharmacy, doctor or non-profit giving it out.
St John vehicles staffed by paramedics carry naloxone here in New Zealand, and there is some broader supply available largely thanks to a swift, one-off ringfenced funding measure put in place during the COVID-19 lockdown last year. As a result, naloxone was able to be purchased by each of the Opioid Treatment Services (OTSs) around the country and in turn distributed to about three quarters of needle exchange clinics.
“This interim supply is welcome and will help reverse overdoses and save lives. However, we have nowhere near the kind of widespread availability we need to deal with the kind of events being witnessed overseas. Even the availability we do have is temporary because the funding source has now closed, and the existing stocks will expire.”
Helm says the situation is a mix of terrifying and baffling.
"We have nowhere near the kind of widespread availability we need to deal with the kind of events being witnessed overseas."
Sarah Helm
Sarah Helm standing by the window with arms crossed. - Sarah Helm, NZ Drug Foundation Executive Director
Usually in these situations an organisation like the Drug Foundation might simply lobby a minister or ministry and garner action that way, but Helm says that primarily it isn’t a lack of support standing in the way, although much more could be being done.
“The main problem is the disjuncture in our health system between the Ministry [of Health], Medsafe, Pharmac, pharmaceutical companies and those who may be able to distribute and/or use, like DHBs, Police and the Needle Exchange or St John.”
A recent report in the International Journal of Drug Policy also said the nation was “grossly underprepared” should an opioid crisis hit.
At a glance: Naloxone availability in Aotearoa
- In 2019, a naloxone nasal spray (Nyxoid) was approved, and was made available for some Crown agencies.
- In 2020, emergency measures were put in place, leading to a limited temporary supply of naloxone in OTSs and about three quarters of Needle Exchanges.
- Also in 2020, an emergency kit containing two Nyxoid nasal sprays was approved for sale without a prescription. However, because it is not funded, at $92 it is out of reach for many people. It is also difficult to source.
- Naloxone ampoules (for injection) continue to be available by prescription-only, which means they can’t be distributed widely to the populations who need them and in most cases are not funded by Pharmac.
- St John vehicles staffed by paramedics carry naloxone, but Police have not yet obtained a supply.
Overseas warnings
Frustration at the failure to get naloxone more freely available has intensified, with concerns New Zealand could face a rapid onslaught of overdose deaths as seen in North America in recent years. In the USA alone, there were 80,000 deaths in the 2019/20 year due to other drugs being laced with fentanyl.
Ben Birks Ang, the Drug Foundation’s deputy executive director programmes, says Canada has also had deaths. “In Canada, people were taking what they thought was MDMA or drugs like that to go out and party, but actually what they were taking was a very, very strong opioid substance and they were overdosing on it.”
A sharp increase in deaths in the space of a few weeks meant the country had to upscale distribution of naloxone quickly and train up a whole group of people on what to do if their friends were overdosing. Birks Ang warns that New Zealand could also face a destructive opioid crisis if the supply of drugs like MDMA and methamphetamine were to be adulterated with extra strong opioids like fentanyl and its analogues.
Just one or two adulterated drug shipments could cause a rapid increase in hospitalisation and deaths among people who weren’t expecting to take a powerful opioid – a situation our current naloxone arrangements leave us poorly prepared for, he says.
“The current situation means we wouldn’t have enough naloxone in the community or the ability to rapidly distribute it if we needed to.”

Naloxone what and why:
Mountain of red tape
Despite the widespread concerns, bureaucracy is getting in the way of making naloxone more available, says Kali Mercier, the Drug Foundation’s policy and advocacy manager.
“The system is heinously complicated”, she says. “It’s a little bit like a Kafka novel because the red tape seems so impenetrable. It shouldn’t be. Naloxone is a harm reduction tool, and we should have been able to get it out to the people who need it by now – other countries simply haven’t had the issues we have had.”
“We had a great step forward when some funding was made available under Covid, which allowed some DHBs to source and distribute naloxone to their OTS clients, Needle Exchanges and elsewhere. But because the regulations are so difficult to navigate, distribution has been very patchy. What we’ve got, while a welcome improvement, only really scrapes the surface of what’s needed in terms of getting this out to all the people and services that need it, training people how to use it, and how to intervene if they see someone who is overdosing. The funding was also just a one-off – there’s no clear way forward for funding this on an ongoing basis.”
Mercier says it feels as if we are set up to fail rather than succeed in getting harm reduction measures in place for those who use drugs. “The Medsafe regulatory and Pharmac funding system hinges on pharmaceutical companies, who are motivated by profit, driving the application process. When the solution to a health issue is likely to be less lucrative – as in this case – the system just doesn’t work.”
Mercier says the Ministry of Health has tried a number of things to push supply forward, but the nation is not significantly closer to getting naloxone out to all the people who need it. Among problems still remaining is that while Nyxoid (the nasal spray) doesn’t need a prescription as part of an emergency kit, it’s expensive and is not funded: “It needs to be [funded] if we want to take disaster preparedness seriously. The kit costs $92 retail. In New Zealand, decisions about funding medicines go through Pharmac. At every turn, there are new hurdles to surmount.”
“Secondly, we need DHBs to be legally able to purchase and distribute emergency kits – at the moment the rules around who can buy them and distribute them seem ‘complicated,’ to say the least.
“Finally, even though Nyxoid nasal spray emergency kits are apparently available as ‘general sales’, when we rang several pharmacies recently, none had even heard of it. They all said their wholesalers didn’t stock it – so it’s not necessarily easily available even when you go hunting for it.”
When the solution to a health issue is likely to be less lucrative – as in this case – the system just doesn’t work.”
Kali Mercier
Kali Mercier head and shoulders - Kali Mercier, NZ Drug Foundation Policy and Advocacy Manager
Hurdles to climb
The Ministry of Health’s chief clinical adviser mental health and addiction, Arran Culver, told Matters of Substance, in written answers to questions, the Ministry had taken significant action to address blocks in improved access over the past few years; but that further availability of naloxone remains reliant on “third parties.”
No third party had applied to Medsafe for prefilled injectable emergency kits, meaning that form of naloxone, used in other countries, was not available. The Ministry was, however, committed to widening the distribution of naloxone.
“Ideally, naloxone would be distributed in emergency kits to people who use opioids and people who could intervene in an overdose situation (for example, family, peers, ambulance paramedics) without a prescription and at no cost.”
Emergency kits, however, must be approved by the Director-General of Health, or their delegate, and there are a number of legislative, regulatory, funding and clinical steps needed to enable this, Culver said.
He was not able to comment on why no third party had registered a pre-filled injectable emergency kit in New Zealand and pointed out Medsafe could not procure medicine applications.
“[Ministry of Health] were advised that an application from a third party for a prefilled injectable kit would be submitted for approval in 2018-2019. Despite support from the Ministry to facilitate this, it did not occur. Addressing this would require a New Zealand [pharmaceutical company] willing and able to source a suitable emergency kit, make an application, and be responsible for importing the kits.”
The nasal spray Nyxoid, however, is available as both a prescription medicine and for general sales in emergency kits. It was approved as a prescription medicine in 2019 and made available to Crown agencies (ESR, Customs and Police) to hold under special permissions to use without prescription, allowing frontline workers to have it in their first aid kits, Culver says.
The Drug Foundation, however, says it appears many of these frontline workers do not know how or when to use it - and a Police spokesperson told Matters of Substance they do not have access to it, “nor are there any plans to change this”.
Culver says Nyxoid is not funded through the Pharmaceutical Schedule and rules prevent DHBs from purchasing, distributing, or using it without Pharmac’s express permission.
Supports in place
When asked why New Zealand is lagging behind other countries in accessing and distributing naloxone, Culver said New Zealand had a different pattern of opioid use due in part to tighter controls on prescribing, which was a factor in preventing the sort of opioid crisis as seen in other countries.
He says there is significant support in place to reduce harm from opioids, such as the DHB opioid substitution services which as of last year supported 5542 people around the country. There is also regular wastewater testing, to measure things like fentanyl, and that information is linked into the Drug Information and Alert NZ network, allowing the Government to intervene if needed and prevent harm. The Drug Foundation says the use of fentanyl for medical purposes can complicate this data.
Culver says the Ministry also works closely with the National Drug Intelligence Bureau and other groups to monitor importation and supply risks.
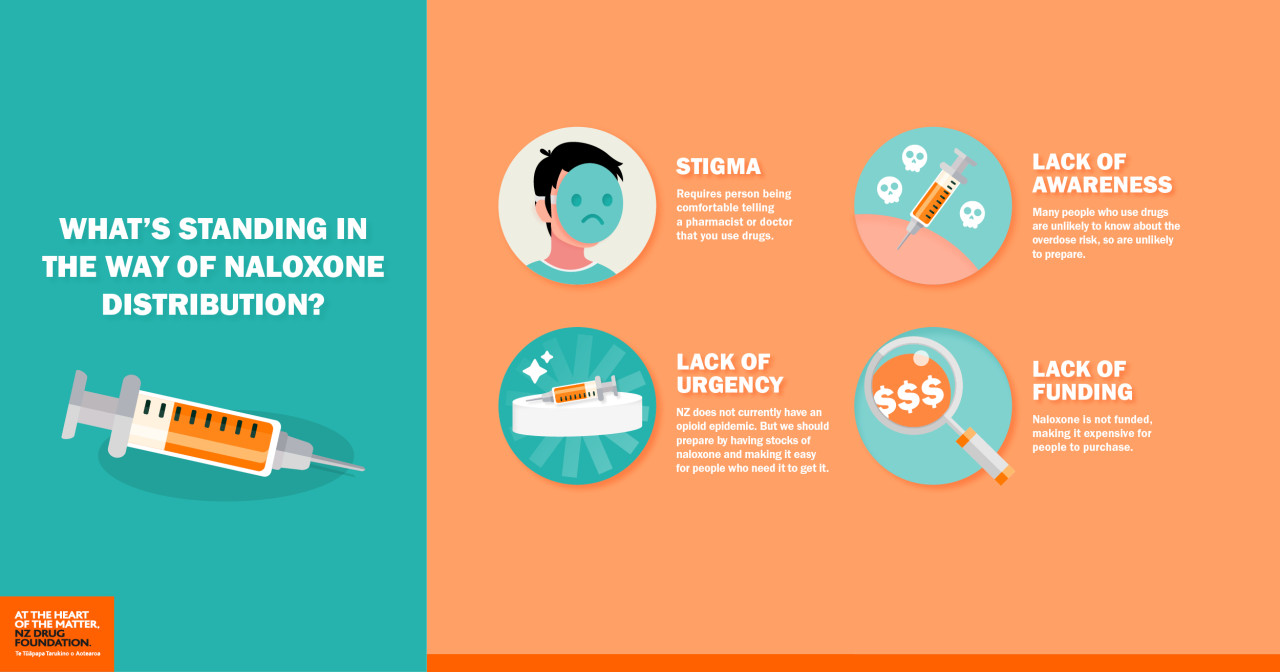
What's standing in the way of Naloxone distribution? Stigma. Lack of awareness. Lack of urgency. Lack of funding.
Other solutions
Jason George, harm reduction lead with the Needle Exchange Programme, has some sympathy for the Ministry which he says has tried to get the drug company to register the emergency kit with the prefilled product, but like others he is frustrated at the lack of progress.
“When the classification of naloxone was changed to allow an approved emergency kit to be distributed without prescription everyone thought ‘great, we’ve done it’ - and yet there is still no action.”
However, while the Ministry told Matters of Substance needle exchanges are not permitted to hold or dispense prescription medicines, 14 out of 20 exchanges are now providing naloxone ampoules or Nyxoid - thanks to Covid-19.
George says because of the lockdowns, many OTSs distributed extra methadone takeaways and supplied naloxone to clients, and also supplied some needle exchanges with naloxone – but not all needle exchanges, due to different interpretations of the regulations by different DHBs.
While that is a positive, George says part of the problem is local outlets have to make individual arrangements with each DHB’s OTS: “Each clinician might have different ideas on if they can/can’t legally supply us, how it should work, the make-up of the packs and so on. For example, in some areas people are supplied with two ampoules (two doses), in others they get five ampoules (five doses).”
George also points out NZNEP clients have used naloxone distributed through the NZNEP to save the lives of friends who were overdosing, and says if a friend of family member of someone who uses opioids came in requesting it, that would be okay, too. “If a person wants naloxone, they do a short training session and can leave with the naloxone in the same visit. It doesn’t take long.”
What we need is a properly funded national solution – legal, consistent, with certainty of supply long-term and easily accessible."
Jason George“To date we have found that the uptake of the naloxone hasn’t been all that high, the last tally was 170 kits total have been distributed across NZNEP outlets that have them. There seems to be a fair degree of apathy amongst people who use opioids in New Zealand when it comes to carrying naloxone.”
George says a better long-term solution is needed that is equitable for all. He points to problems with inconsistency of supply to outlets, different interpretations of regulations, and the regulations themselves which lead to uncertainty. “We really don’t know how much is available and for how long.” Exchanges need to be able to supply naloxone without worrying about it being stopped, or getting in trouble due to regulations.
While his preferred product would be an emergency kit with prefilled syringes, he also says that given the problems around getting such a kit registered, an alternative might be to give up on that product and instead fund the nasal spray.
Another option would be to change the classification of the ampoules to make them available without prescription and ensure some level of training around how to use them.
“The ampoules are probably the least desirable option when compared to the Prenoxad (prefilled syringe) or Nyxoid (nasal spray) options, but ultimately better than nothing.
“What we need is a properly funded national solution – legal, consistent, with certainty of supply long-term and easily accessible for everyone – opioid users and their friends/family and anyone who is likely to encounter an opioid overdose or be around people who use opioids. Ideally, it would be available from all needle exchange outlets, OTSs and pharmacies, or needle exchange pharmacies.”
Just get it out there
George says the situation is urgent. He and Rhys Ponton, from Auckland University’s School of Pharmacy, wrote to the New Zealand Medical Journal last year about Pharmac changing a morphine product leading to a powdered opioid scene in New Zealand – and that is a big concern.
“We don’t traditionally have a lot of heroin in New Zealand and when you have a powdered drug scene it does lend itself to that drug being cut by something like fentanyl and other impurities.”
Birks Ang wants Nyxoid kits to be funded and the regulations clarified so that DHBs can legally purchase and distribute them. He also wants a distribution plan in place as soon as possible.
Julian Buchanan, retired academic and long-time harm reduction specialist, doesn’t care much which product it is as long as naloxone gets out and available in the drug using community.
“In Australia… they’ve got outreach workers who are wandering the streets dishing out naloxone and this is a general approach in many other countries.”
Buchanan blames institutional discrimination against people who use banned drugs as being the main issue holding up resolution – “that’s the backdrop of this and that can’t be sidestepped.”
But many people who use banned drugs have serious pre-existing issues – they may have been abused, in care, fostered, or have learning difficulties and some could be suicidal or homeless.
Those people get referred to as junkies or drug seekers by the medical profession and they don’t attract much attention in terms of resources and of priorities.”
And there are consequences to admitting opioid use - someone Buchanan knows was admitted to hospital in agony after breaking a bone, but when the person told staff he used drugs they stopped giving him opioids for his pain.
Buchanan also wants a ‘good Samaritan’ law brought in to end potential arrest for helping a person who uses drugs, saying he knows of another person who took someone overdosing to a phone box, called an ambulance, and ran away in case the Police also arrived and arrested them.
Naloxone, Buchanan says, is a “miracle drug” that saves lives and is harmless. Just like other life-saving equipment, we need to have it available: “There’s somebody dying every week of this - this is a life-saving issue. It’s a no-brainer.”
Recent news

Reflections from the 2024 UN Commission on Narcotic Drugs
Executive Director Sarah Helm reflects on this year's global drug conference
What can we learn from Australia’s free naloxone scheme?
As harm reduction advocates in Aotearoa push for better naloxone access, we look for lessons across the ditch.

A new approach to reporting on drug data
We've launched a new tool to help you find the latest drug data and changed how we report throughout the year.

