New study shows therapeutic cannabis' benefits and barriers

How effective is medicinal cannabis at helping New Zealanders manage pain, anxiety, and other conditions? And how easy is it for people to get their hands on? A new study, led by Associate Professor of Criminology at Victoria University, Dr Fiona Hutton, alongside Dr Geoff Noller from Otago University, sought to find out.
CW: this story mentions suicide.
The study looked at New Zealanders’ experiences accessing and using cannabis for medicinal purposes. Two hundred and thirteen participants with medically diagnosed conditions such as chronic pain or anxiety were recruited through ‘green fairies’ - a colloquial term referring to people who provide medicinal cannabis on the black market to those in need, and an Auckland cannabis clinic. Participants answered a 36-question survey and took part in semi-structured interviews.
The research team were interested in medicinal cannabis’ influence on users’ symptoms, side effects, and issues related to its accessibility and cost. The team also explored cannabis’ impact on user relationships and the quality control of product purchased through the black market.

Dr Fiona Hutton
Medicinal cannabis is legal, but access remains difficult
It’s been more than three years since the scheme aiming to make medicinal cannabis more accessible came into effect. However, due to it being expensive and requiring people to navigate a somewhat complicated process, many New Zealanders still get their product from the illicit market, particularly via green fairies. NZ Drug Foundation analysis in 2022 estimated that more than 250,000 New Zealanders were still accessing medicinal cannabis via the black market.
Dr Hutton says part of her motivation for doing the study was to get people’s stories about therapeutic use of cannabis out there and ultimately, gather evidence and to advocate for change. She says of the work green fairies do: “[They] risk a lot to ease people’s pain and suffering because of the way the law stands.”
Who are the green fairies?
Dr Hutton says it was clear from the research that “[Green fairies] have got a huge amount of knowledge and respect in the community, and they’ve been advocating for change for decades.”
The fairies who participated in the study described to the research team that the products they provided mostly had names, labels, and proper instructions about how to take them.
While most people interviewed in the study had good experiences with green fairies, some of the interviewees talked about “green goblins,” a term describing supposed fairies who “sell people shit – and say it’s medicinal,” Dr Hutton says.
Study findings
An overwhelming 95.6% of participants in the study reported positive effects of cannabis in managing their conditions, with the top three benefits being pain relief, improved sleep, and anxiety reduction.
Other findings from the study included:
- Cannabis dramatically improved symptoms of serious conditions like seizures and chemotherapy side effects, prompting a need for more research into its therapeutic uses.
- The general wellness of users also saw significant improvement, with reports of enhanced energy levels and improved relationships.
- The study highlighted certain negative effects like difficulties in managing doses, cognitive impairment, and stress from sourcing cannabis from illegal markets. Despite this, these effects were characterised as "relatively minor" and were often mitigated by adjusting dosage or the THC/CBD mix.
Dr Hutton said she had expected the results to be more mixed and was surprised the feedback they got was so consistent.
“I was quite stunned by the overwhelming positivity, and how cannabis had helped people with a variety of conditions,” she says.
Some people spoken to in the study had been suicidal before starting medicinal cannabis, telling the research team they couldn’t stand taking pharmaceuticals anymore.
People were saying things like “medicinal cannabis saved my life, it’s changed my life, it’s a miracle,” Dr Hutton says.
An alternative to conventional medicine
Nearly all participants in the study had been through the health system and most had unsatisfactory experiences. This led to almost all of them turning to the illicit market and green fairies.
A key finding from the study was that with the introduction of therapeutic cannabis, participants decreased their use of other prescribed medications, especially opioid-based ones. Dr Hutton described that due to having fewer side effects and risks of dependence, cannabis proved to be a promising alternative for many patients.
However, the research paper called for a balanced approach for NZ, noting that conventional medications may still be necessary for some patients.
“We're not saying that there's no place at all for conventional medicine – clearly these medications are helpful for some people,” Dr Hutton says.
In the wake of the results of her study, Dr Hutton felt “very frustrated” with the existing medicinal cannabis scheme and the reluctance of some doctors to prescribe.
“We have this plant-based medicine, which is not really addictive in the form that it's given out to people.”
“Why don’t we start with this first, instead of just going ‘right, here’s some tramadol?’” she says.
The difficulty of accessing medicinal cannabis through official means
The difficulties in accessing legal medicinal cannabis in NZ have been well documented. Dr Hutton says the system makes “the brain ache” because “it seems so ridiculously overcomplicated.”
The study found that one of the major barriers to accessing medicinal cannabis was cost, with currently available medicinal cannabis products being too expensive for many New Zealanders. Depending on the product someone wants, it can cost hundreds of dollars to fulfil a prescription. Sativex, a cannabis-based medicine used to treat multiple sclerosis symptoms of muscle stiffness and spasms, currently costs around $1000 a month.
Dr Hutton said another barrier for access to medicinal cannabis is that some GPs can be reluctant to prescribe. “If [patients] have sort of chronic conditions, then they're often in contact a lot with their GP. And GPs can be reluctant to suggest it.”
She believes most GPs are well intentioned and don’t want their patients to come to harm for something they’ve prescribed, and while many GPs are supportive and willing to prescribe cannabis, there is still significant stigma around its use.
Conclusion and recommendations
The authors argue that at present the system not working as it should. Given the inconsistent quality of products on the illicit market, the study recommends the government makes therapeutic cannabis products more accessible and available for those who might benefit.
At present, the law allows terminally ill people an exemption to possess and use illicit cannabis. The researchers say that this exemption should be broadened. They propose decriminalising the use, possession, and cultivation of cannabis for medical purposes to improve access. They also emphasised the potential of incorporating green fairies into the healthcare system legally, arguing for the importance of Real-World Evidence (RWE) in shaping future policies and practices concerning therapeutic cannabis use.
Dr Hutton also argues that increasing funding for legal cannabis products could encourage a shift away from pharmaceuticals.
Despite the study's limited scope, the overwhelmingly positive outcomes suggest that expanding the accessibility of therapeutic cannabis could benefit many New Zealanders.
Dr Hutton concludes that although NZ has a legal medicinal cannabis system, it was clearly not working for those interviewed for her study, many of whom were in desperate need and suffering from chronic, often painful conditions.
“We need to do something different now. Please! Let's just get on with it... Can we get on and stop pussyfooting around and tinkering around the edges? Let’s be bold!”
Recent news
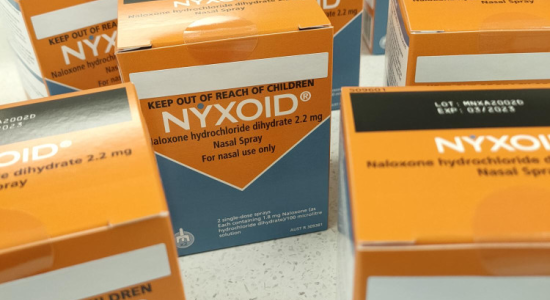
Expert Pharmac committee recommends funding for overdose reversal nasal spray
Public funding for a lifesaving opioid overdose reversal nasal spray is one step closer, with an expert committee saying that funding the medicine for use by non-paramedic first responders and people at high risk of an opioid overdose is a

Reflections from the 2024 UN Commission on Narcotic Drugs
Executive Director Sarah Helm reflects on this year's global drug conference
What can we learn from Australia’s free naloxone scheme?
As harm reduction advocates in Aotearoa push for better naloxone access, we look for lessons across the ditch.

